SBPMD Histology Laboratory Manual
Hematopoiesis & Bone Marrow
The red marrow of adult human bones is the major site of formation of erythrocytes, granulocytes, monocytes and platelets. Some lymphocytes are formed in the bone marrow as well. Lymphocytes will be studied with lymphoid tissue.
There are stem cells that are precursors of both the red and white blood cell series. These undifferentiated cells have been identified and studied by special techniques in research laboratories, but their proportion in bone marrow is low. Therefore, it is unlikely that you will be able to recognize them in your slides. (Do not spend time looking for stem cells).
The student should bear in mind that the frequency of any given cell type or stage of differentiation in the marrow is a complex function related to the relative frequency of the cells in the blood, to the turnover time or half life of the cell type in the circulation, and to the maturation time of the cells in the marrow. The most frequent precursor series is the erythroid cell series with the neutrophilic series being the second.
Distinctions between the cells of the granulocytic series are based on nuclear morphology and the size and staining properties of the granules. Oil immersion is required for this type of determination. Criteria for evaluating cell type and stage of maturation are as follows: Size of the cell and its nucleus. In general there is a gradual decrease in size of the cell and its nucleus with maturation. However, remember that cells preparing to undergo mitosis enlarge before division; so depending on size alone can be misleading. Also some cells may be flattened out on the slide more than others during preparation of the smear.
Appearance of the chromatin network in the nucleus. Immature cells have a delicate fine-meshed chromatin network. More mature cells have coarser, more condensed chromatin.
Presence or absence of nucleoli. Nucleoli are visible as pale blue circular areas within the chromatin network of immature cells.
Cytoplasmic basophilia. Very immature cells have pale blue cytoplasm, due to the presence of only a few scattered ribosomes.
Specialized cell products. Accumulation of hemoglobin in erythroid cells, and the appearance of granules and their type in granulocytes.
Erythroid Series
- Proerythroblast - Finely meshed chromatin in nucleus, generally two prominent nucleoli, cytoplasm moderately basophilic, due to the presence of ribosomes. An unstained region indicating the location of the Golgi apparatus is often visible.
- Basophilic erythroblast - This cell is usually smaller and the nucleus, which is intensely heterochromatic, is centrally located. The cytoplasm is a deeper blue color than that of the proerythroblast, due to the mixture of abundant free ribosomes and the initiation of hemoglobin synthesis. There is no longer a visible Golgi apparatus.
- Polychromatophilic erythroblast - The nucleus is intensely heterochromatic, and the cytoplasm is now a characteristic lilac color. The basophilia is due to the cytoplasmic ribosomes, and the acidophilia is due to the increase in the amount of hemoglobin being synthesized by the ribosomes. This is the last stage during which cell division occurs.
- Normoblast (orthochromatic erythroblast) - The nucleus has become pyknotic and therefore is very dark in appearance. The abundant cytoplasmic hemoglobin is acidophilic.
- Erythrocyte (RBC) - The extrusion of the nucleus from normoblasts results in the formation of anucleate erythrocytes. Occasionally there is still some residual basophilia in the cytoplasm of these cells, due to the retention of some ribosomes. Such immature red cells are called reticulocytes (after staining by cresyl blue) because of the so-called reticulated pattern of cytoplasmic basophilia. A small percentage of reticulocytes enter the circulation normally before completing their maturation. However, when there is a great increase in erythrocyte production, there is an increased percentage of reticulocytes entering the blood, and reticulocyte counts can provide information about the rate of erythrocyte production.
Granulocytic Series
Stem cells that differentiate into the granulocytic series give rise to the myeloblast, a large cell with a large ovoid pale-staining nucleus, 2 to 5 nucleoli, and lightly basophilic cytoplasm (due to a scattering of ribosomes). These cells are difficult to distinguish, but see demonstration of myeloblasts in peripheral blood from a patient with acute myeloid leukemia.
- Promyelocyte: This large cell is very similar to a myeloblast, but can be distinguished from the latter by the presence of a few azurophilic granules (pinkish-purple, primary lysosomes) in its cytoplasm.
- Myelocyte: The promyelocyte in turn gives rise to eosinophilic, neutrophilic and basophilic myelocytes, which have both azurophilic and specific granules according to their respective cell line. These cells can be identified by the round nucleus and by the accumulation of specific granules in their cytoplasm.
- Metamyelocytes: This stage can be identified by the indented nucleus and the presence of their specific cytoplasmic granules. You may be able to identify the unstained image of the Golgi complex in the region where the nucleus is indented. In the neutrophilic lineage, the late metamyelocyte is called the band cell.
- Mature granulocytes: The mature cells can be recognized by their complex nuclear morphologies and their specific granules. Do not confuse the fine granules of the neutrophil (which may appear lightly acidophilic) for the coarser granules of eosinophils or basophils. The highly lobulated nucleus of the mature neutrophil is helpful in its identification.
#82, Human Bone Marrow Smear (Wright's stain)
Open with WebViewer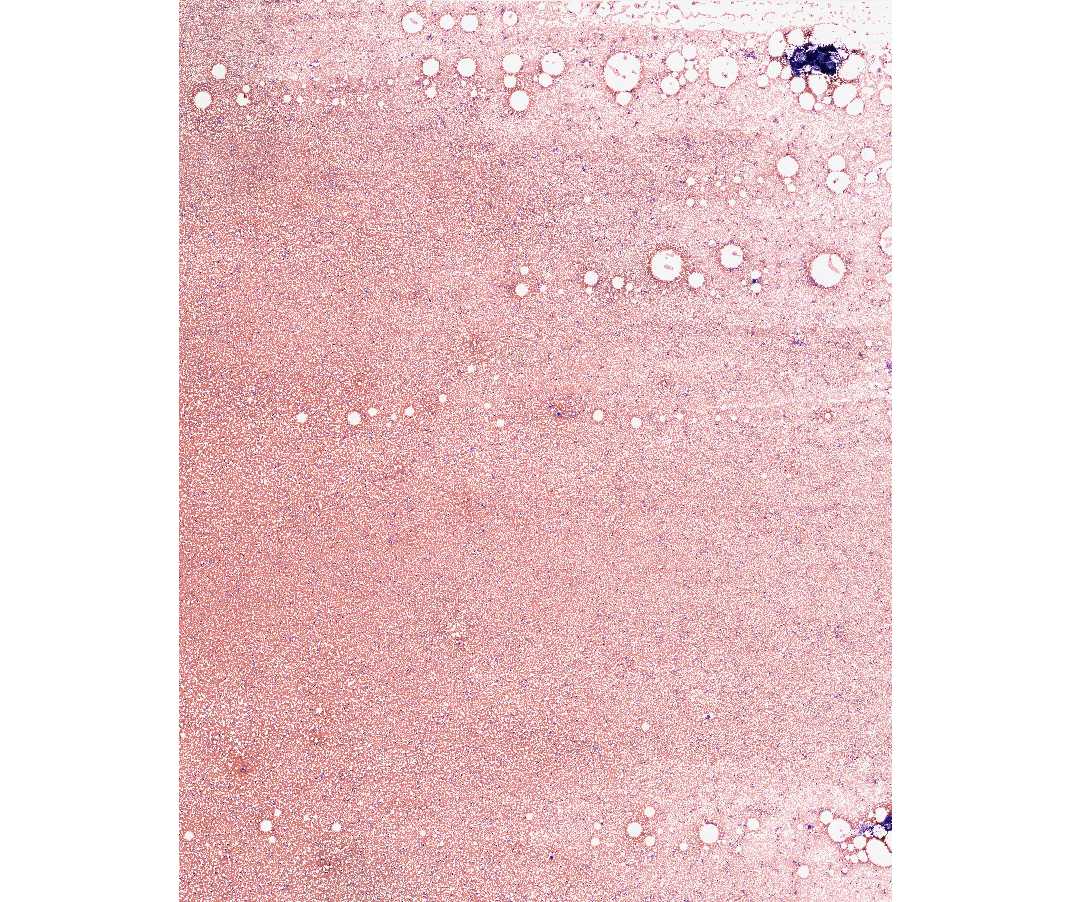
The textbook and handout should be reviewed before an attempt is made to identify the precursor stages of myeloid differentiation on this slide. The slide should be scanned under low magnification. The most immediately obvious cell type will be the enormous megakaryocyte which gives rise to blood platelets. An area of this slide where the cells are not too closely smeared should be chosen. Study the cells of the erythroid and granulocyte series.
The following points should be kept in mind when examining bone marrow smears:
1. You will be unable to identify all cells in the smear.
2. You should be able to assign a well-fixed and well-stained cell to either the erythrocyte or granulocyte line of development.
3. You should be able to say whether a cell is relatively undifferentiated (i.e., not far removed from the stem cell) or nearly, or completely, differentiated.
4. If a cell in the granulocyte line already has specific granules it should be further classified into the neutrophilic, eosinophilic, or basophilic series and based on its nuclear morphology, whether it is a myelocyte, metamyelocyte, or a mature cell.
Be sure you know the biochemical composition of the cytoplasmic granules of neutrophils (polymorphonuclear leukocytes) and eosinophils.
#52, Bone marrow, Human, core biopsy, H&E
Open with WebViewer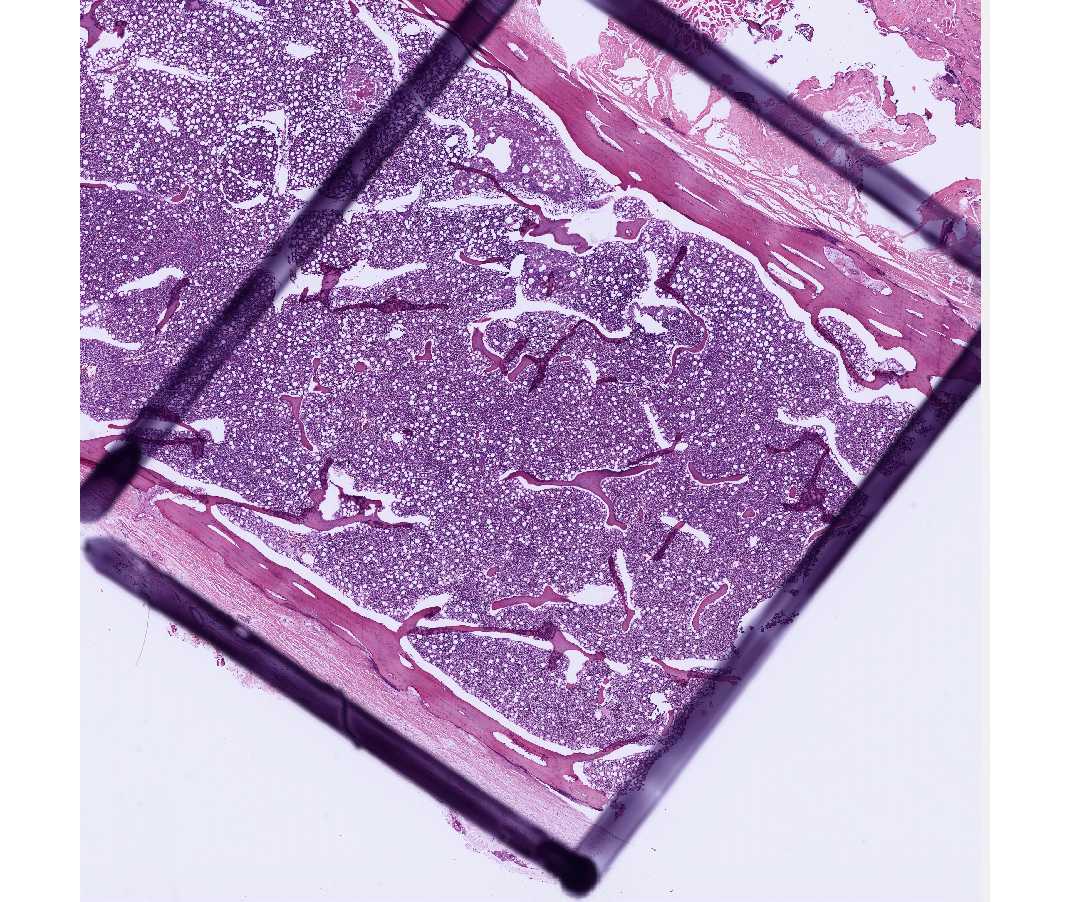
This is a bone marrow core biopsy. Note the spicules of bone and intervening marrow. The marrow is approximately 60-70% cells and 30-40% fat. Note the conspicuous megakaryocytes and areas of erythroid and myeloid development.
#14, Bone marrow, section, Rabbit (Giemsa)
Open with WebViewer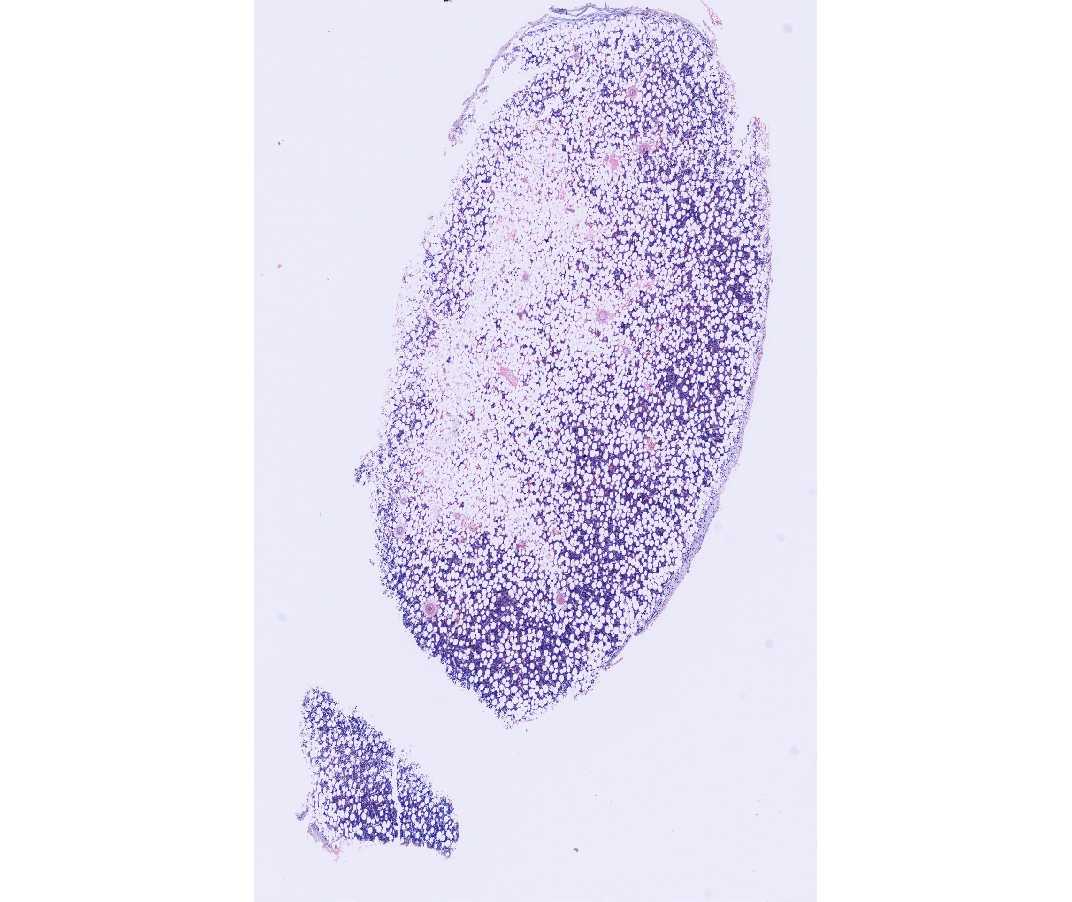
Like the section of human bone marrow, this also reveals the natural relationship of developing blood cells to one another and to sinusoids. Note the megakaryocytes and the developing red and white blood cells. The cells of the erythroid and myeloid series tend to be grouped in small foci and that within each group the cells tend to be at the same stage of development. Variable amounts of adipose tissue are present.