Columbia Doctors:
Mental Health
Background
New
York Quality Care (NYQC), the Medicare Shared Savings Program (MSSP)
Accountable Care Organization (ACO) affiliated with the outpatient faculty
practices of NewYork-Presbyterian (i.e., ColumbiaDoctors, Weill Cornell
Medicine, NewYork-Presbyterian Medical Group) has piloted a collaborative care
model (CoCM) that integrates the management of depression into the primary care
setting (Exhibit 1). The CoCM pilot is part of a broader effort by NYQC to
improve its depression screening rates, which lag the national average
generally, and other academic medical centers in the New York region more
specifically, according to annual reporting provided by the Center for Medicare
and Medicaid Services (CMS).
The
CoCM is currently centrally-funded by the CoCM, but as it scales, will need to
become a financially self-sustaining program. Thus, the primary objective of
this project was to determine the expected financial impact of the CoCM as an
independent program, and identify strategies to improve its financial self-sustainability
as it scales.
Project approach
In
order to address the questions laid out by ColumbiaDoctors and NYQC, we
conducted this project over two phases:
1.
Phase
1: Identify
the ‘base case’ configuration and impact
During
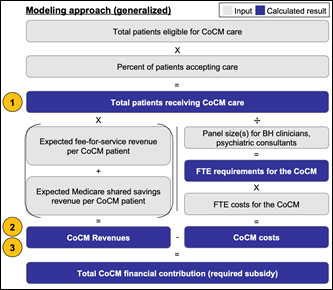
this phase, we developed a quantitative methodology, shown in Exhibit 2, to
estimate the financial impact of the CoCM, and conducted both (a) secondary
research and (b) interviews with stakeholders from across NYQC to collect the
inputs necessary to forecast the CoCM’s estimated annual financial impact
through 2026
2.
Phase
2: Produce
and prioritize options for financial improvement
In the
second phase of the project, we reviewed the model methodology to identify
levers for improving the net impact of the CoCM, quantified the impact of each
of these levers through a model sensitivity analysis, and worked with
stakeholders at NYQC to prioritize each of these improvement opportunities in
terms of feasibility. Then, we leveraged interview feedback with NYQC
stakeholders to identify tactics to drive improvement in these prioritized
areas.
Key findings
Although
the CoCM is expected to operate at a loss through the end of the forecast
period, this loss is relatively modest, and is expected to diminish as the
model reaches scale (i.e., more patients are screened for depression and
‘screen into’ the CoCM). The estimated financial loss may even be offset by the
potential shared savings incentives generated through the MSSP, although these
benefits will be difficult to directly attribute to the CoCM.
The
primary levers through which to improve financial sustainability include
improving the depression screening rate, improving patient acceptance of CoCM
care, capturing additional opportunities for coding, and dynamically adjusting
CoCM staffing to meet patient demand. The most feasible levers to affect are
improving the depression screening rate, and improving patient acceptance of
CoCM care, which can be activated primarily via patient and provider education.
Closing Thoughts
The
benefits of better screening and management of behavioral health conditions has
been well-documented, and models for affecting outcomes such as the CoCM have
been in existence for many years. However, financing these models continues to
be a challenge, and improving these models’ financial sustainability and
ultimate efficacy require both changing physician behavior and addressing
broader societal stigma around mental health care. We look forward to seeing
ColumbiaDoctors and NYQC continue to evolve this model to better serve
patients.
Exhibits
Exhibit
1: Schematic of
the Collaborative Care Model
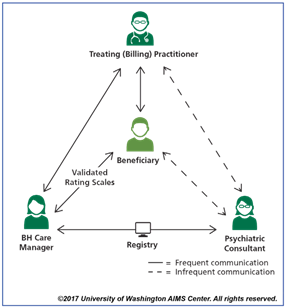
Exhibit 2: Model Methodology