Harnessing
the Power of Telemedicine in a Non-Pandemic World
Telemedicine has proved to be an
integral tool during the COVID-19 pandemic. As health care Providers begin
pandemic recovery and think about patient care in a non-pandemic setting, how
can Providers continue to best utilize this highly effective tool and fully
recognize its benefits in a changed environment?
Photo credit: National Cancer Institute; free to use under the Unsplash License.
Project
Objective
Through the Columbia Business
School and the Vagelos College of Physicians and
Surgeons masterclass, Healthcare Management, Design and Strategy, the Columbia Business School Student
Team collaborated closely with ColumbiaDoctors’
Digital Health Executive Committee to address a fundamental business problem:
how can ColumbiaDoctors further expand telemedicine
adoption to increase practice revenues in a non-pandemic world?
The
primary objective of the project is to develop a robust telemedicine adoption
strategy for ColumbiaDoctors to effectively increase
practice revenues. According to current practitioners, telemedicine visits
generally require half the amount of time as the exact same type of in-person
visit. Given this finding, there is a significant opportunity to increase the
total number of billable visits through increased telemedicine adoption and
conversion of clinically appropriate in-person visits to telemedicine visits.
Telemedicine affords the large urban practice to increase revenue without
requiring drastic operational changes or increased capital expenditures.
Furthermore, favorable reimbursement and payment parity to in-person visits
fortify the rationale to drive telemedicine adoption to increase revenues.
The primary
project goal was to first identify the best approach to increase telemedicine
adoption and then subsequently deliver a strategic resource that ColumbiaDoctors can leverage to execute on the selected
approach. In using the choice structuring approach, we aligned on the following
three options, of which we selected a single strategy to move forward with:
Solution Approach – Choice structuring, Options
Option 1: ColumbiaDoctors will default all non-acute visits to
telemedicine, assuming the visit does not require immediate in-person attention
(e.g., physical procedure).
Option 2: ColumbiaDoctors will require each individual physician to
conduct a certain percentage of patient visits via telemedicine.
Option 3: ColumbiaDoctors will require each subspecialty to conduct a
certain level of telemedicine (i.e., high, medium, low).
Recommendation
After assessing ColumbiaDoctors’ telemedicine usage data (before, during,
and through the public health emergency), patient satisfaction data, and
interviewing various members of the Digital Health Executive Committee, we
decided that “Option 3” was the best strategic approach to increase
telemedicine adoption. Through stakeholder interviews, it is evident that
physician satisfaction’s correlation with telemedicine utilization varies quite
significantly among individual physicians (and between subspecialties). In
turn, this variability is a key factor impacting overall telemedicine adoption.
By holding the responsibility of increased adoption at
the subspecialty level (as opposed to the individual physician as in Option 2),
telemedicine usage can be tailored to the needs of individual physicians within
the subspecialty as well as across the subspeciality overall.
After aligning on Option 3, the
Telemedicine Assessment & Adoption Tool was developed to help
subspecialties identify individualized ways to increase
telemedicine adoption. This tool is intended for pilot use by subspecialties in
the surgery department. From there, ColumbiaDoctors
can assess its adoption effectiveness and tailor it to serve other departments
in the practice.
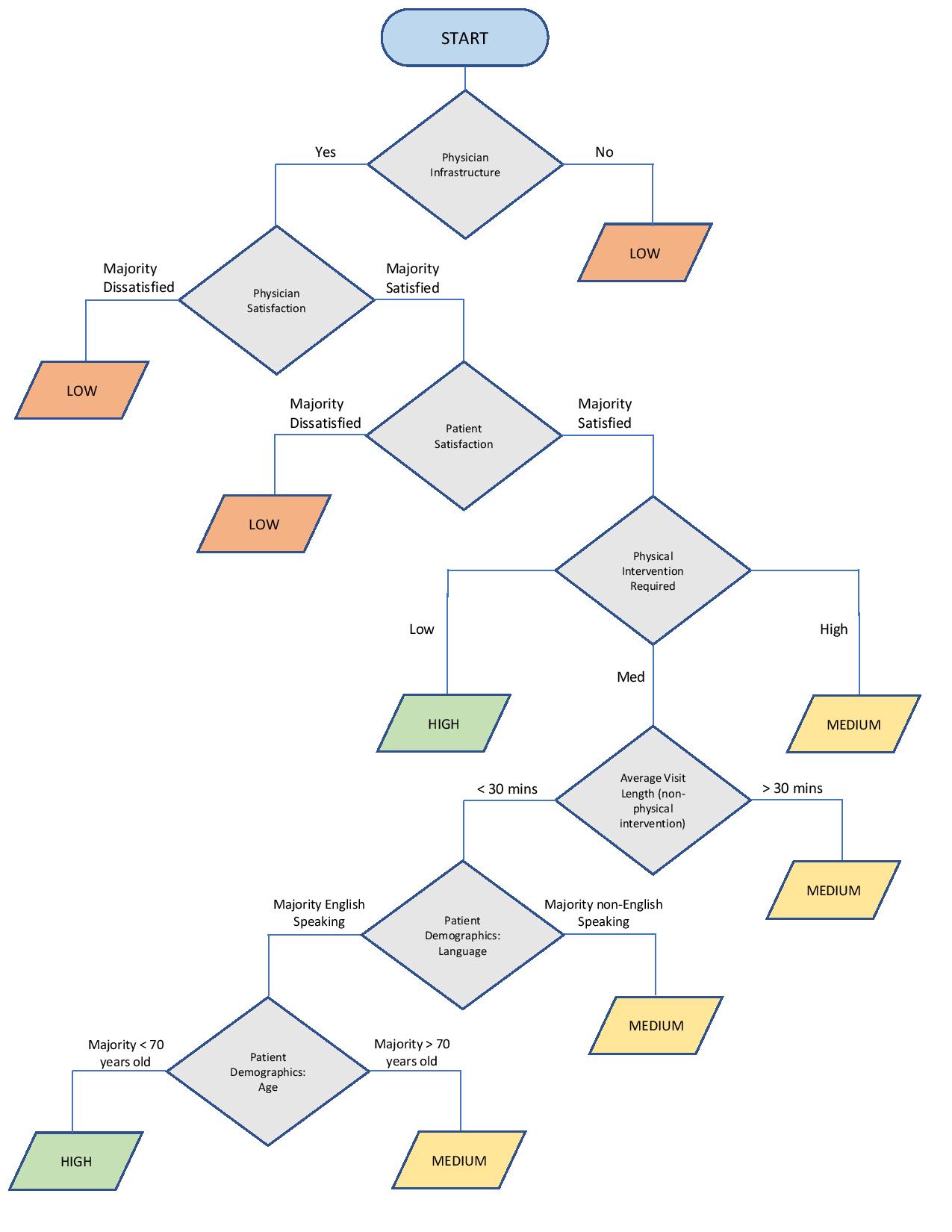
The Telemedicine Assessment
& Adoption Tool has 3 key sections: the
Assessment Tree, Recommendations, and Benefits/Opportunities. The Assessment Tree is a guided flowchart that the subspecialty
Leader can use to assess the subspecialty’s potential level of telemedicine
adoption, which the tool characterizes as High, Medium, or Low. A High level of
potential adoption would mean that telemedicine could be a key tool for the
subspecialty to deliver care, regularly used alongside necessary in-person
visits without disruption to the existing clinical workflow (i.e., majority of
visits conducted virtually). A Medium level of potential adoption would mean
that there is an opportunity to integrate telemedicine into the current
clinical workflow; however, specific operational and clinical constraints
prevent a High level of adoption at this time (i.e., some/many visits conducted
virtually but not the majority). A Low level of potential adoption is defined
as little to no telemedicine utilization with the potential to overturn
operational constraints and increase adoption.
The Assessment Tree generates either a High, Medium, or Low level for potential
adoption based on key criteria that can have a significant impact on adoption.
The seven criteria are physician infrastructure (e.g., portal access, IT),
physician satisfaction, patient satisfaction, degree of physical intervention,
average visit length, patient language, and patient age. Again, these are
assessed at the subspecialty level (not individual patient level). The tool
also includes detailed instructions for how to assess each criterion.
Based on the subspecialty’s
output from the Assessment Tree, the Recommendations section provides
suggestions for how the subspecialty can increase adoption. For example, if the
output is Low due to low patient satisfaction with telemedicine (as assessed
via previously collected data), the tool suggests the following:
"Understanding the root of the patient dissatisfaction is important. If the team is unable to survey patients,
encourage staff to ask patients for feedback and personal assessment of
telemedicine for anecdotal evidence. Dissatisfaction may come from access/IT
issues, quality of care, or the attending physician. Many of these may prove
addressable (e.g., ensuring Doximity backup is used,
providing better communication on wait-times, using the virtual waiting room,
providing feedback, and coaching physicians on virtual care).”
The final piece of the tool
includes the numerous Opportunities and Benefits of increased telemedicine
adoption, including reduced patient wait times, extension of patient reach,
etc. Importantly, a model is also leveraged to illustrate the rationale for how
increased telemedicine adoption can increase practice revenues using the
colorectal department within surgery as a specific case study. In brief, given
various assumptions on pricing, payment parity, and visit length, the model
shows that just a 1% increase in telemedicine adoption within colorectal
surgery could lead to increased annual revenues of well over $50,000. Across
the entire specialty, this would amass to millions of dollars in increased
revenue.
Final
Thoughts
The COVID-19 pandemic rapidly
accelerated the uptake of telemedicine and provided a strong proof of concept
for the telehealth industry. Harnessing the power of telemedicine beyond the
pandemic may give certain practices a competitive edge, and, if deployed
effectively, will likely lead to increased revenue, higher patient satisfaction,
practice efficiencies, and more. Of course, changes in reimbursement policies,
payment parity, and licensing could create barriers to telemedicine
utilization; however, given the current landscape and resounding success of
telemedicine during the pandemic, telemedicine appears here to stay for the
foreseeable future. ColumbiaDoctors is leading the
way towards new standards in health care through effective expansion of the use
of this tool, and we look forward to seeing the positive impact that further
telemedicine adoption can deliver through the ColumbiaDoctors
Team.
Contributors: Minyoung Choi, Skyler Cohen,
Prerana Katiyar, Claire Nishioka