Simulation Modeling on the Impact of testing and PPE on Provider Availability
By Carri W. Chan, Columbia Business School and Kuang Xu, Stanford Graduate School of Business
About:
We were interested in understanding the impact of the personal protective equipment (PPE) shortage and limited testing on provider availability. In turn, we estimate what this would mean for the number of patients who can receive treatment. Our interest was to provide some quantification of the sentiment that if we cannot protect our healthcare workers, they will not be able to work and provide much needed care. This is critical because in a recent study of a public health emergency in need of mechanical ventilators, staff is projected to be bottleneck. This study serves as the basis of recommendations from the Society of Critical Care for the COVID19 pandemic as well as the basis of our analysis.
Methodology:
· Simple simulation model based on epidemiological models and national data to understand implications of PPE and testing on staffing availability
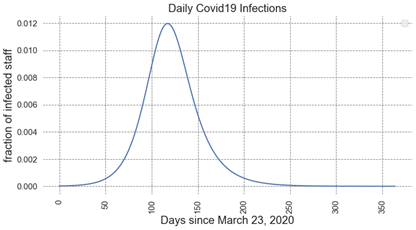
o COVID19 infection model – based on SIR model
§ Main assumptions:
· Death rate: 2%, recovery rate 98%
· Reproduction number R0=2
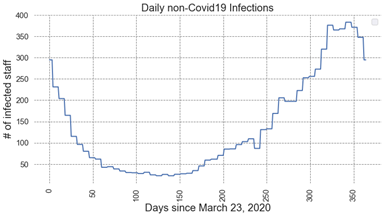
o Non-COVID19 infections (e.g. cough/cold) – based on historical data
§ Seasonal trajectory taken from the 2018-2019 influenza data by CDC
· https://gis.cdc.gov/grasp/fluview/fluportaldashboard.html
· Extrapolated from weekly counts
§ About 1B common cold in the US
· https://medlineplus.gov/commoncold.html
§ Assumes an annual total of 35.5m infections in the US (about 10% of population)
· https://www.cdc.gov/flu/about/burden/2018-2019.html
· https://www.cdc.gov/flu/about/keyfacts.htm
§ Assumes healthcare staff contracts the disease with the same likelihood as the national average
· Varied testing capabilities
o Considered scenarios where 30%, 50%, 70%, or 100% of symptomatic providers are able to be tested.
§ We use 30% testing as a baseline.
o In the absence of a test, and symptomatic provider must self-quarantine (not work) for 14 days.
o 98% of providers with a positive test can return to work within 14 days. The remaining 2% never return to work
· Varied impact of PPE availability
o Considered scenarios where PPE availability reduces the risk of infection by 10%, 25%, 50%, and 100%.
§ While most clinicians believe that full PPE would reduce the risk of infection on the job to 0%, there is still the chance of infection through community spread, so we consider full PPE availability to reduce risk by 50%.
§ If providers use make-shift PPE, including using bandanas, we assume this reduces the risk by 25%. We use this number as our baseline.
Results:
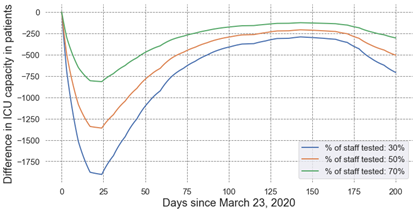
 Impact of Staff Testing
Impact of Staff Testing
Our estimates suggest that ICU capacity would drop by 1,900 patients by April 15, 2020, if we could only test 30% of symptomatic providers instead of 100%
Impact of PPE availability
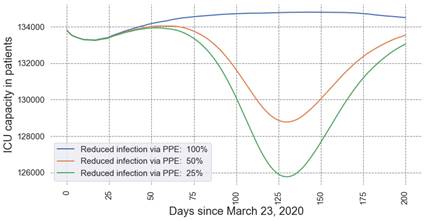
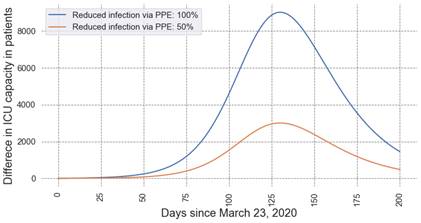
Our estimates suggest that ICU capacity would drop by up to 3,000 patients at the time of peak infections with partial PPE that can only reduce the risk of infection by 25% versus PPE that can reduce the risk of infection by 50%. If full PPE could really completely eliminate the risk of provider infection, only having PPE which could reduce risk by 25% risk would reduce ICU capacity by over 9,000 patients.
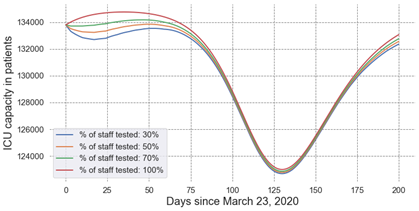
Joint testing and PPE availability
We compared Scenario 1 of 30% testing of symptomatic providers and 25% reduction in risk due to partial PPE to Scenario 2 of 100% testing of symptomatic providers and 50% reduction in risk due to PPE. We also assume an 8 day ICU Length-of-stay. Over the next 200 days (starting from March 23), we estimate this would result in over 45,000 more patients that could be treated in Scenario 2 versus Scenario 1.
Conclusions
Our frontline employees are risking their own health and safety to care for the influx of COVID19 patients. Limited testing and PPE availability puts our healthcare providers at more risk and limits their ability to continue to provide care. The current shortage of testing and PPE could result in unavailability of 5% of our providers! We need to prioritize our providers and provide the resources for them to continue to do their jobs safely and effectively.