 |
|||||||||||

|
|||||||||||
 |
|||||||||||
| The Harriet and Robert Heilbrunn Department of Population and Family Health |
|||||||||||
 |
|||||||||||
|
intro | reproductive anatomy and physiology | contraception | pregnancy, childbirth and lactation |
|||||||||||
SECTION II:
|
|||||||||||
| Introduction | Hormonal Methods |
| Non-Hormonal Methods | Other Methods |
| Emergency Contraception |
Introduction
Sixty-one percent of all women worldwide who are within the reproductive age (15-44 years old), are using methods of contraception (methods used to deliberately prevent pregnancy). These estimates vary by region:
- In developed countries, 69% of women use methods of contraception, yet in developing regions it is only 59%.
- Only 27% of reproductive aged women in Africa use a method.
- 64% of reproductive aged women in Asia, and 71% in Latin America and the Caribbean use a method.
- The most commonly used methods worldwide are female sterilization (21%), the I.U.D. (14%), and oral contraception (7%).
- Women in more developed countries are more likely to use short-acting and reversible methods, such as oral contraceptives and condoms.
- Women in less developed countries are more likely to use female sterilization and I.U.D.s.
- According to the National Surveys of Family Growth (NSFG), released in 2002, 93% of U.S. women of reproductive age (15-44) who are at risk of pregnancy are using some type of contraceptive method. 2
Over the past 10 years, contraceptive use has increased in developing countries; however there is still a high unmet need for family planning services.3,4
In many parts of the developing world, contraception remains either unavailable or limited. Even in the United States, where many women can choose from a variety of methods, almost half of all pregnancies are unintended.5
These unintended pregnancies are almost evenly divided between pregnancies due to non-use, and pregnancies due to contraceptive failure.
No method of contraception is 100% effective other than complete abstinence from sexual intercourse. However, many methods exist that are close to 100% effective if used consistently and correctly. People frequently fail to use their method every time or to use it perfectly. Thus, even people using a method may face an unintended pregnancy. Factors contributing to unintended pregnancy are complex, and may involve the interplay of emotional, psychosocial, political, religious, cultural, and economic forces.
The standard of care mandated in U.S. federally-funded family planning programs (Title X) includes non-judgmental counseling that is culturally sensitive, age appropriate, and offered with respect for a woman's right to confidential services.
Applying this standard of care, public health practitioners provide information, support, and counseling about contraceptive use, enabling women to make informed decisions. Public health practitioners also play important roles in designing, implementing, and evaluating programs to promote pregnancy prevention in communities, refugee camps, schools, and through the media..
This section provides an overview of the most commonly used contraceptive methods by category: hormonal methods, non-hormonal methods (including emergency contraception), and permanent methods. Each method is described as follows:
- How the method works to prevent pregnancy (mechanism of action);
- How the method is used;
- Effectiveness;
- Advantages/Disadvantages; and
- Importance of Dual Method Use (for prevention of sexually transmitted infections).
Contraceptive effectiveness rates are estimates of the probability that a pregnancy will occur during the first year of method use. Perfect use refers to the effectiveness of a method when it is used consistently and correctly. Typical use refers to the effectiveness of a method for the average person who does not always use the method correctly and consistently.
Hormonal Methods
Many hormonal birth control methods utilize a combination of hormones (i.e. synthetic estrogen and progestin). Other methods contain only one hormone (progestin).
Combination Hormonal Methods
Oral contraceptive pills (OCPs), the Ortho Evra Patch, and the NuvaRing prevent pregnancy by:
- Preventing ovulation by blocking the LH surge;
- Inhibiting sperm penetration by thickening the cervical mucous;
- Delaying sperm transport; and
- Limiting the sperm's ability to fertilize the egg.
Oral Contraceptive Pills

Source: U of Maryland
Method Use
- The pill is taken daily at about the same time for 21 days, followed by a hormone-free period of seven days, during which a withdrawal bleed that resembles a menstrual period takes place (accompanied by either taking no pills or seven placebo pills).
- Other options for use of birth control pills include taking two, three, or four consecutive cycles of 21 pills (up to 84 active pills) followed by one seven-day hormone free interval.
- If more than one or two pills are missed, women should use a back-up method for the remainder of that pill pack and until they have ingested seven active pills in a row in order to remain protected from pregnancy.
Effectiveness
- High (99.7% with perfect use).
Potential Benefits/Advantages
- Not coitus dependent (i.e. does not need to be used at the time of intercourse).
- Decreases dysmenorrhea (pain associated with menstruation), menstrual blood loss, and pre-menstrual symptoms.
- Reduces incidence of ovarian cysts, benign breast conditions, pelvic inflammatory disease, uterine fibroids, and iron deficiency anemia.
- Reduces risk of ectopic pregnancy,
- Reduces risk of endometrial and ovarian cancer, although not of breast cancer.
- May improve acne.
Disadvantages/Risks
- Must be taken daily around the same time, so is not a good method for people who would have trouble doing that or don’t want family members to know they are using birth control.
- May be expensive for women who do not have insurance coverage for contraception or access to free or low cost services.
- Provides no protection against sexually transmitted infections including HIV.
- Cardiovascular events, i.e. heart disease, stroke, and venous thromboembolism (blood clots), although extremely rare, do occur at increased rates. Women with known risk factors for cardiovascular disease (such as smokers) are at increased risk.
- Absolute contraindications (medical conditions precluding use of the method) include blood clotting disorders, heart disease, uncontrolled hypertension, severe migraine headaches, major surgery with prolonged immobilization, breast, endometrial or other estrogen related cancers.
Dual Method
- Condoms should be used for first seven days for contraceptive protection, and on-going for STI/HIV prevention.
Warning Signs/Major Side Effects
Warning signs that a woman may be developing the major side effects of birth control pills (rare cardiovascular complications) are:
A = Abdominal Pain
C = Chest Pain
H = Headaches (severe)
E = Eyes (i.e., blurred vision, loss of vision)
S = Severe leg pain (blood clot in the legs)
Minor Side Effects
Minor side effects of the birth control pill may include nausea, appetite changes, breast tenderness, and/or spotting or bleeding between menstrual periods. Although they usually resolve within one to three months, and do not pose health risks to women, minor side effects may result in method discontinuation.
Educational Messages
1. Teaching women about the possibility of very common minor side effects when initiating the pill and other combination methods can help allay fear and increase compliance.
2. Conditions that contraindicate the use of the pill and other hormonal birth control methods are not common in the majority of women of childbearing age. The risks of developing serious problems with hormonal method use are low. Yet, a survey conducted in 2000 revealed that 41% of women interviewed thought that the pill was associated with significant health hazards.6 Therefore, advising women on the relative safety and effectiveness of the pill and other hormonal methods of birth control is important.
Contraceptive Patch

Approved in 2002, the patch is a small adhesive strip that is applied to the skin (administered transdermally), permitting hormones to enter the bloodstream directly.
The effectiveness, mechanisms of action, advantages, disadvantages, major and minor side effects, warning signs, and dual methods are similar to the oral contraceptive pil.
Method Use
- The patch is applied anywhere on the body except for the breasts, the palms of the hands, or the soles of the feet.
- One patch is applied each week for three weeks on the same day, also called, “Patch Change Day.”
- During the fourth week, no patch is used (this is called the “patch-free week”). A withdrawal bleed usually occurs during the patch-free week.
- Consider use of emergency contraception if patch is off for more than one or two days and unprotected sex occurs.
Additional Potential Benefits/Advantages
- An important advantage of the patch is that the woman does not need to remember to take a pill each day.
- Because hormones enter the bloodstream directly, bypassing breakdown in the liver, the possibility of gastrointestinal side effects (i.e. nausea and vomiting) is decreased.
Additional Disadvantages/Risks
- Skin irritation at the site of placement is found in approximately 20% of patch users.
- Less effective in women over 198 pounds.
Vaginal Ring

Approved in 2002, the NuvaRing is a soft, flexible ring that releases a low and steady amount of estrogen and progestin, which are absorbed into the blood stream through the vagina.
The effectiveness, mechanisms of action, advantages, disadvantages, major and minor side effects, warning signs, and dual methods are similar to the oral contraceptive pill.
Method Use
- Use of the ring generally requires comfort with self-insertion.
- The ring is inserted in the vagina but placement doesn’t matter as long as it is secure. Because it is placed in the vagina, some people are confused and think it provides some type of physical barrier, which it does not.
- Following insertion, the ring is left in place for three straight weeks, and removed after 21 days, to allow for a ring-free week when a withdrawal bleed usually occurs.
- Consider use of a back-up method such as condoms or emergency contraception if ring is out of the vagina for more than three hours, or if the new ring is not re-inserted on time.
- For a video about the insertion and use of the NuvaRing, go to:
http://www.youtube.com/watch?v=eA-KbuxXGvo
Additional Potential Benefits/Advantages
- After insertion, the woman does not need to remember to take a pill each day.
Progestin-Only Hormonal Contraceptives
Progestin-only methods provide options for women who cannot use estrogen, and for women who are breast-feeding.
Depo Provera, Noristerat, the mini-pill, Norplant, and Implanon prevent pregnancy by:
- Inhibiting ovulation by suppressing FSH and LH, and eliminating the LH surge.
- Thickening the cervical mucous and preventing sperm penetration.
- Producing changes in the endometrial lining.
The Mirena I.U.D. ( see I.U.D. section, below) also contains progestin.
Depo Provera
(depot medroxyprogesterone acetate/DMPA)
Method Use
- Usually injected within the first seven days of menstruation, though a quick start protocol is a more promising prevention strategy.
- The woman returns for injection every 11-12 weeks (3 months).
- Consider a back-up method such as condoms or emergency contraception if late for injection.
Effectiveness
- Highly effective method of birth control (99.7% with perfect use).
Benefits/Advantages
- Not coitus dependent.
- Rare cardiovascular effects of methods containing estrogen have not been demonstrated.
- Decreases dysmenorrhea and menstrual cramping.
- Reduces risk of ectopic pregnancy, anemia, endometrial cancer, uterine cancer, and pelvic inflammatory disease (PID).
- Safe option for breast-feeding women.
- Does not affect fertility long-term.
Disadvantages/Risks
- Delay of return to baseline fertility (average is about 10 months) may occur. However, pregnancy risk is immediate if re-injection is late.
- Provides no protection against sexually transmitted infections including HIV.
- Unpredictable menstrual patterns, including either increased spotting and bleeding or amenorrhea (absence of menstrual periods).
- Weight gain.
- Breast tenderness.
- Decrease in bone density, which probably reverses upon discontinuation (further study of the long-term effects of Depo Provera on bone density, particularly in adolescents is needed).
- Depression in individual women but not overall.
- Inability to immediately discontinue method.
- Rare allergic reactions.
Warning Signs/Major Side Effects
- Repeated, very painful headaches
- Heavy Bleeding
- Depression
- Severe lower abdominal pain
- Pus or prolonged pain or bleeding at the injection side.
Minor Side Effects
- Irregular bleeding patterns
- Amenorrhea (loss of periods)
Dual Method
- Condoms should be used for first seven days for contraceptive protection, and on-going for STI/HIV prevention.
Noristerat
Used primary in Latin America and Africa, Noristerat's effectiveness, mechanisms of action, advantages, disadvantages, major and minor side effects, warning signs, and dual methods are similar to Depo Provera.
Method Use
- Injection every two months
Progestin Only Pills (“Mini-Pills”)
The mechanisms of action, advantages, disadvantages, major and minor side effects, and warning signs, are similar to those of Depo Provera.
Mini-Pill Method of Use
- Usually begins with menses, or post-partum while breast-feeding.
- Take one pill daily at the same time. If three hours late for pill, back-up method is needed.
- Consider a back up method such as condoms or emergency contraception for incorrect or inconsistent use.
Effectiveness
- High (99% with perfect use)
- Slightly less effective than combined hormonal pills
Additional Disadvantages/Risks
- Very important that method be taken every day at the same time of day.
- Expensive for women who do not have insurance coverage for contraception or access to free or low cost services.
- Pregnancy is more likely than with the regular pill when pills are missed due to the low dosage.
- Delayed period after several months after pill discontinuation may be a sign of pregnancy
Norplant and Implanon Implants
In the United States, the use of Norplant was discontinued in the late 1990's, but it is still used in over 60 countries. Implanon, a new progestin-only implant, is available in Europe and now the United States.
The mechanisms of action, advantages, disadvantages, major and minor side effects, and warning signs are similar to those of Depo Provera.
Method Use:
- Through a minor surgical procedure, six rod implants (Norplant) or one rod implant (Implanon) are implanted under the skin in the upper arm.
- The rod implants release a daily dose of levonorgestrel.
- Can be used for up to seven years.
Effectivness
- Very effective method (99.5% with perfect use).
Additional Disadvantages/Risks
- Dependent on a medical provider for method removal, which can be a barrier if experienced providers are not readily available.
Non-Hormonal Methods
The diaphragm, cervical cap, male condom, female condom and sponge prevent pregnancy by:
- Creating a “barrier” between the sperm and the ovum.
Diaphragm
The diaphragm is a dome-shaped rubber cup that is inserted into the vagina before sexual intercourse

Photo courtesy of CBAS
Method Use
- Spermicidal (sperm-killing) jelly is applied inside of the diaphragm before it is inserted.
- The diaphragm is inserted up to six hours before intercourse, and must be left in place for six hours following intercourse.
- If intercourse is repeated, additional spermicide should be inserted into the vagina with an applicator without removing the diaphragm.
- For more detailed information about how to insert a diaphragm, go to:
http://www.webmd.com/sex/birth-control/tc/diaphragm-use-and-care-topic-overview
Effectiveness
- Diaphragm effectiveness with perfect use is 94%. With typical use, it is 80%.
Benefits/Advantages
- There are few medical risks associated with the diaphragm
Disadvantages/Risks
- In rare instances, users report irritation or allergy from the spermicide.
- The only major side effect of using the diaphragm is toxic shock syndrome (TSS), a rare but serious disorder caused by the staphylococcus aureus bacterium. The risk of TSS is very low among barrier method users (three cases of per year can be expected for every 100,000 women using vaginal barrier methods, resulting in one death for every 100,000 users).
Cervical Cap
The cervical cap is a small rubber cup that fits snugly onto the cervix.
Method Use
- Prior to insertion, spermicide is placed inside the cap. Additional spermicide is not needed for repeated intercourse. The cap can be left in place for up to 48 hours. Cap use longer than 48 hours is not recommended (increased risk of TSS).
Effectiveness
- Effectiveness of the cap is 74% with perfect use and 60% with typical use.
Disadvantages/Risks
- Limited sizes of cervical caps are available in the U.S. which means that some women will not be able to be fitted for the cap. Additional sizes are available in other developed countries.
STI Protection: Although the latex male condom is the best method of preventing the transmission of STIs and HIV, other barrier methods such as the diaphragm and cervical cap may provide some STI/HIV protection as well. Studies in both the United States and developing countries are investigating the use of barrier methods and newly formulated microbicides (microbe killing creams or jellies) in the reduction of STI/HIV transmission risk.
Sponge
The sponge is a small, soft, and round piece of polyurethane foam that contains spermicide and is inserted into the vagina before sexual intercourse.
Method Use
- Before inserting it into the vagina, the sponge should be wet with a small amount of water to activate the spermicide.
- The sponge is inserted so that it covers the cervix and positioned with the nylon loop at the bottom for easy removal.
- The sponge protects for up to 24 hours, even with repeated intercourse, and must be left in place for at least six hours after intercourse. It should not be worn for more than 30 hours due to increased risk of TSS.
- The sponge can be used only once and should be discarded in a waste receptacle and not the toilet. Effectiveness
- Sponge effectiveness with perfect use for women who have never given birth is 91%. With typical use, it is 84%.
- Sponge effectiveness with perfect use for women who have previously given birth is 80%. With typical use, it is 68%.
Benefits/Advantages
- The sponge is available without a prescription and can be inserted up to 24 hours before sex.
Disadvantages/Risks
- The sponge contains nonoxynol-9, a spermicide that can cause irritation to the vaginal tissue, increasing susceptibility to STIs including HIV.
- There is also a small risk of toxic shock syndrome (TSS), a rare but serious disorder caused by the staphylococcus aureus bacterium. The risk of TSS is very low among barrier method users (three cases of per year can be expected for every 100,000 women using vaginal barrier methods, resulting in one death for every 100,000 users).
Condoms
Male and female condoms will be described below. Because both prevent pregnancy by blocking the passage of semen into the vagina, they also prevent STIs and HIV.
Male Condom

Male condoms are available in latex, lambskin, and/or polyurethane. All three materials effectively prevent pregnancy. Lambskin contains small pores that may permit the passage of bacteria and viruses, and are thus not recommended for infection prevention.
Method Use
- New condoms must be used with each act of intercourse.
- Check expiration date of the condom.
- If penis is uncircumcised, pull back foreskin before placing the condom, if possible.
- Gently pinch the tip of the condom to squeeze out air to allow room for the semen.
- Place condom on erect penis before intercourse by carefully unrolling it all the way down to the base of the penis.
- Make sure condom is being unrolled in the right direction (if condom does not unroll, it is probably in-side out).
- Use adequate lubrication (only water-based lubricants should be used with latex condoms, because oil based lubricants – creams, oils, petroleum jelly, etc. – may cause latex to tear).
- After ejaculation, withdraw the penis from the vagina before the penis becomes flaccid, and hold the rim of the condom against the base of the penis to prevent the semen from spilling.
- Do not flush condoms in toilets as they will clog plumbing.
Effectiveness
- Male condom effectiveness is 98% with perfect use, and 85% with typical use.
Advantages/Benefits
- Provides protection against both pregnancy and STI/HIV.
- Widely accessible without a prescription.
- Causes almost no medical side effects.
Disadvantages/Risks
- Coitus dependent.
- Reduced sensitivity for men however, this may be an advantage for preventing premature ejaculation..
- Some men have difficulty maintaining erections, especially when they are inexperienced condom users.
- Challenge to use in relationships where there is weak partner cooperation and/or intimate partner violence or coercion.
- Latex allergy.
STI Prevention: When used consistently and correctly, condoms prevent the transmission of HIV and other sexually transmitted infections. Despite prior evidence that using a spermicide containing nonoxynol-9 along with condoms decreases the risk of STIs and HIV, this is no more effective than using a condom with non-spermicidal lubricants (water based only). In fact, recent studies have indicated that nonoxynol-9 may actually increase the risk of HIV transmission during vaginal sex.8
Female Condom
The female condom is a polyurethane sheath - one end is inserted into the vagina while the other remains outside of the vagina and provides some protection to the external genitalia. It contains a silicone lubricant. Additional lubricant is provided with each condom.
Female Condom Use
- Inserted up to eight hours before intercourse.
- With the thumb and middle finger of one hand, squeeze the inner ring (at the closed end of the pouch) into a narrow oval. With other hand, spread the vaginal lips and insert the inner ring and the pouch into the vagina and push it gently high up into the vagina. An outer ring rests on the outer lips of the vagina. During intercourse, the penis should be guided into the pouch through the outer ring.
- Following ejaculation, the penis should be removed from the vagina, while holding onto the female condom.
- To remove condom, first twist the outer ring, and pull the condom out gently.
- Use a new condom with each act of intercourse.
Effectiveness
- Female condom effectiveness is 95% with perfect use, and 80% with typical use.
Advantages/Benefits
- Dual protection against pregnancy, and STI/HIV.
- Accessible without prescription
- Causes few medical side effects
- Some people find female condoms to be more comfortable and less constricting than male condoms, as they are wider.
Disadvantages/Risks
- Coitus dependent
- More expensive than male condoms
- Challenge to use in relationships with weak partner cooperation and/or intimate partner violence.
Other Methods
Intrauterine Device (I.U.D)
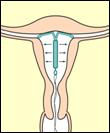
The Intrauterine Device (I.U.D.) is a small, t-shaped device that is inserted into the uterus to provide reversible and long-term protection against pregnancy. Worldwide, approximately 106 million women use the I.U.D.9
The two most commonly available I.U.D.'s are the:
- Mirena (which releases progestin, and is also known as the LNG-IUS levonoregestrel-releasing intrauterine system);
- Copper T 380 (aka Paraguard). Internationally other copper I.U.D.'s are also available (i.e. TCu-220C, TCu-200C, the Nova T, and the Multiload 375).
I.U.D.'s prevent pregnancy by:
- Preventing sperm from fertilizing ova by affecting the way sperm move and inhibiting sperm’s ability to reach and join with an ovum.
- Altering the lining of the uterus, which may make it more difficult for implantation to occur.
- The Mirena has a method of action that resembles that of other progestin-only hormonal methods. That is, the progestin prevents ovulation and also causes the thickening of cervical mucous, both or which prevent pregnancy.
Method Use
- I.U.D.'s can be inserted by a medical professional any time during the month, if medical providers are reasonably certain that the woman is not pregnant, and if current or recent upper reproductive tract infections are ruled out.
- Women must assure correct placement and check for signs of infection by going for medical follow-up six weeks following insertion.
Effectiveness
- Highly effective with rates ranging from 99.3-98.8%.
Advantages/Benefits
- Not coitus dependent
- Long term (up to 10 years with the Copper T and five years with the Mirena).
Disadvantages/Risks
- Provides no protection against sexually transmitted infections and HIV.
- Potential cramping and pain with insertion.
- Menstrual irregularities (i.e. heavier menses with the Cu T380, and irregular but light bleeding or spotting during the first few months with the Mirena)
- Expulsion (2-10%) of women will expel within the first year.
- Perforation of uterus (uncommon and usually related to the skill of person inserting device).
Dual Method
- Condoms should be used for ongoing STI/HIV prevention.
Withdrawal (Coitus Interruptus)
The withdrawal method for pregnancy prevention refers to when a man pulls his penis out of his partner’s vagina before ejaculation so that he does not ejaculate inside his partner.
Withdrawal prevents pregnancy by:
- Preventing sperm from entering the vagina (and thus the uterus and fallopian tubes) and fertilizing an ovum.
Effectiveness
- In terms of pregnancy prevention, withdrawal effectiveness is similar to that of the male condom. Effectiveness is 96% with perfect use, and 82% with typical use.
- Consider back-up method such as emergency contraception if ejaculation begins before withdrawal.
Advantages/Benefits
- Withdrawal requires no money, devices, hormones, or medical provider, making it available to anyone.
Disadvantages/Risks
- Provides no protection against sexually transmitted infections and HIV.
- Requires a great degree of self-control. For some men, it may be difficult to ensure that they withdraw before ejaculation has started.
- For some people, pleasure may be diminished by the interruption of sexual intercourse.
Permanent Contraception
Surgical sterilization provides permanent contraception to both women and men. It is an important option for persons who are certain that they do not want more children. Effective counseling is crucial to assure that men and women considering these procedures are fully comprehend the permanence. Sterilization does not provide protection against STI/HIV.
Female sterilization is the most widely used contraceptive method. Worldwide, 21% of women aged 15 to 49 use female sterilization11, which is a surgical procedure that involves blocking or cutting the fallopian tubes to prevent fertilization. It is safe, with mortality rates at 1-2 deaths per 100,000 as compared to maternal mortality rates of 7.9 deaths per 100,000 live births.12
Male sterilization (vasectomy) blocks the vas deferens and therefore prevents the passage of sperm into the semen. After having a vasectomy it takes between 15-20 ejaculations to have sperm-free semen. Other forms of contraception should be used until semen is confirmed to be sperm-free.
Vasectomy is simpler and safer procedure than female sterilization and may be reversible, though fertility return is not guaranteed.
Fertility Awareness/Natural Family Planning
Fertility awareness methods rely on understanding the most likely time that ovulation will take place during the monthly cycle, so that intercourse is avoided, or a barrier method is used. Fertility awareness methods include:
- The Standard Days Methods
- The Calendar Rhythm Method
- The Symptothermal Method
- The Ovulation Method
The effectiveness of fertility awareness methods range from 98% with perfect use, to 78% with typical use. Although an important option for women worldwide, fertility awareness methods overall are less effective than other methods. Male partners must be continuously cooperative. Physiologic changes (i.e. recent childbirth, current breast-feeding, early menstruation, discontinuation of other hormonal methods, approaching menopause) can affect reliability.
Emergency Contraception
Emergency Contraceptive Pills
The emergency contraceptive pill (ECP) is an important pregnancy prevention option for women in cases when contraception failed, was not used, was used incorrectly, and in cases of non-consensual intercourse.
ECP has often been referred to as the “morning after pill,” however it is effective in preventing pregnancy if taken within 120 hours of unprotected sexual intercourse.
ECP is not an abortifacient (that is, it is not a process or substance that induces an abortion). ECP prevents pregnancy by preventing or delaying ovulation, interfering with fertilization, and/or preventing implantation (similar to other hormonal contraceptives).
There are currently two types of pills marketed specifically as emergency contraception: progestin-only ECP (Plan B), and combination estrogen and progestin ECP (Preven). Where both ECP formulations are available, practitioners recommend Plan B. It is more effective than combined ECP (89% reduction in pregnancy, compared to 75%), and it rarely produces the nausea and vomiting that may be associated with combined ECP.
Emergency contraception alone is not considered a primary method of birth control, because it is not as effective as other methods. However, repeated use of emergency contraception is not harmful.
ECP eligibility should be assessed at all reproductive health visits, and, if the woman is eligible, it should be provided along with a highly effective birth control method for ongoing use.
ECP is widely available for purchase over the counter in urban areas. In much of the developing world, however, education about appropriate use is often lacking. The use of ECP in some regions of the world may be related to the lack of availability of adequate family planning services.
IUDs as Emergency Contraception
Emergency contraception can also be obtained through the insertion of a copper IUD within five days of unprotected intercourse. This method is an excellent option for women who are interested in using the IUD an as on-going method of contraception. The copper IUD is about 99% effective in preventing pregnancy after unprotected intercourse.

61% of all women worldwide, who are within the reproductive age (15-49 years old), are using methods of contraception. |
Teaching the acronym “ACHES” is a “gold standard” of family planning education. |

