 |
|||||||

|
|||||||
 |
|||||||
| The Harriet and Robert Heilbrunn Department of Population and Family Health |
|||||||
 |
|||||||
|
intro | reproductive anatomy and physiology | contraception | pregnancy, childbirth and lactation |
|||||||
SECTION III:
|
|||||||
| Introduction | Pregnancy |
| Childbirth | Breastfeeding and Lactation |
Introduction
Effective public health practice leading to healthy mothers and infants depends in part upon basic knowledge about pregnancy, prenatal care, safe labor and delivery, and breastfeeding.
Pregnancy
Signs and symptoms which may alert women, and their health care providers, to the possibility of pregnancy include: a missed menstrual period, nausea and/or vomiting, increased frequency of urination, fatigue, breast tenderness, and/or mood changes.
Often, medical providers confirm suspected pregnancy, usually by conducting a pregnancy-related history, performing a urine pregnancy test, and/or conducting a physical examination. In addition, many women use highly sensitive over-the-counter pregnancy tests.
Learning of a positive pregnancy diagnosis, a woman may feel immediate, intense emotion, ranging from complete joy to utter despair. When a woman’s reaction is one of confusion or conflicting emotions, she may be unsure of her next steps, and seek information from her medical provider and/or public health practitioner.
Professionals who deliver pregnancy test results and/or Pregnancy Options Counseling should provide each woman with comprehensive information in a sensitive and non-judgmental manner (regardless of the age and life circumstances of the individual) so that she may weigh the range of clinical options and make her own decision.
Stages of Pregnancy
A full-term pregnancy is considered to last 40 weeks from the first day of the pregnant woman's last menstrual period (LMP) prior to fertilization. Pregnancy is generally divided into trimesters:
- First Trimester – the first 12 weeks of pregnancy in which embryonic and early fetal development takes place.
- Second Trimester – the 13-27th weeks of pregnancy.
- Third Trimester - the 28-40th weeks of pregnancy.
Fertilization, the fusion of the male sperm with the female ova in the fallopian tube to form a single cell called the zygote. Once formed, the rapidly dividing zygote travels towards the uterus (which takes about three days). Transport is facilitated by ciliated epithelium (epithelium are hair-like structures that wave actively in one direction) and subtle contractions of the fallopian tube.
When the zygote reaches the uterus it has become a blastocyst (a small cluster of cells) that remains in the uterus for four or five days before it penetrates into the thickened endometrium (uterine lining). This process, called implantation occurs approximately 10 days after fertilization and marks the beginning of the embryonic period (development which occurs during the first eight weeks of pregnancy).
The Implanted Blastocyst (Maria Wawer Slide)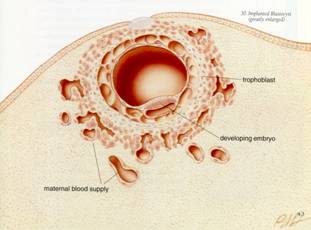
The American College of Obstetricians and Gynecologists (ACOG) defines the beginning of pregnancy at the completion of implantation into the lining of the uterus.13
First Trimester
For the first eight weeks post-fertilization, and ten weeks from the last menstrual period (LMP), the cells are termed an “embryo.” After eight weeks post-fertilization and ten weeks from LMP until birth, the term changes to “fetus.” During the first trimester, the embryo is the most susceptible to environmental influences; during this stage, the majority of organ system formation occurs.
THE DEVELOPING PLACENTA
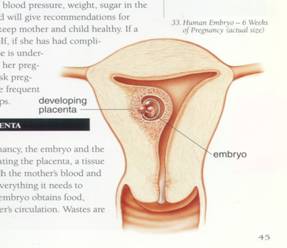
During the early stages of embryonic development, a thin membrane called the amnion develops, which surrounds and protects the embryo. The membrane contains amniotic fluid, which cushions the fetus and helps to maintain even temperature throughout pregnancy.
The outer cells of the embryo form projections, called “villi” that attach themselves to the uterine wall. This attachment becomes the placenta, a vascular spongy structure through which the embryo, and later the developing fetus, derives oxygen, antibodies and nutrients from the maternal blood supply. Waste products also pass from the fetus back to the maternal blood supply through the placenta. The embryo is connected to the placenta by the umbilical cord.
Soon after implantation, the placenta secretes a hormone called HCG (human chorionic gonadotrophin). HCG prevents the disintegration of the corpus luteum, which will secrete large quantities of estrogen and progesterone. Increased estrogen production also causes the enlargement of the uterus, breasts, and external genitalia. Increased progesterone helps to maintain the endometrium, prevents uterine contractions during the pregnancy, and prepares the breasts for lactation.
By the end of the fourth week, all major organ systems begin to form. Primitive nervous system development begins with the neural tube (the beginnings of the brain and the spinal cord). The cardiovascular system also begins to develop. The heart begins beating during the 4th week, and limb buds (which eventually become the arms and legs) also develop by the fourth week. By the end of eight weeks, all major body systems (circulatory, nervous, digestive and urinary systems) continue to develop and function.
Additional Information
1. HCG is secreted into the urine of a pregnant woman, and is the basis of most commercial urine pregnancy test kits. Along with history and physical examination, HCG is used to diagnose pregnancy.
2. Studies indicate that about 50-70% of neural tube defects (NTDs) could be prevented if women obtained sufficient amounts of folic acid before becoming pregnant and during pregnancy. There is a higher incidence of NTDs among females (60-70% female), and there are ethnic, geographic, and environmental differences.14
3.Because the neural tube forms in the very early stages of embryonic development, initiating folic acid after pregnancy diagnosis is too late. Women who could become pregnant should get 400 micrograms of synthetic folic acid each day, or eat food enriched with 100% of the daily value of folic acid.15
The end of the first trimester marks the beginning of the fetal period (from 9-12 weeks), and is characterized by continued structural growth and development of the major organ systems and the external genital organs.
Exposure or ingestion of environmental or chemical toxins (e.g. x-rays, certain drugs and/or infections, environmental pollutants) can result in congenital malformation, impaired growth or fetal death. The early diagnosis of pregnancy therefore can alert women and their health care providers to avoid exposures to potential teratogens (substances which cause the development of abnormalities in an embryo or fetus).
Second Trimester
The second trimester occurs during weeks 13-27 and is marked by accelerated growth, the development of reflex responses and muscular activity. The placenta is fully developed and the brain undergoes the most important period of growth.
Third Trimester
The third trimester begins at week 28 and continues until the birth of the baby. All major organ systems continue to grow and mature including the brain, the kidneys and the lungs. By approximately the 36th week, the fetal head may “drop” into the pelvis, a process called lightening. The fetus is considered full-term at >= 37 weeks. It weighs approximately 3000-3600 grams, unless small for gestational age (SGA).
Additional Information
1. Gestational age and fetal weight determine infant survival chances if labor begins early. According to the 2002 ACOG Guidelines, survival prior to 24 weeks gestation is extremely rare and the likelihood of survival increases with time. The guidelines note that the survival rates increase from 0% at 21 weeks gestation to 75% at 25 weeks gestation; and from 11% at 401-500 grams to 75% at 701-800 grams birth weight. Long-term follow-up studies are being conducted to assess the degree of increased risk for cognitive and neurological deficit with younger and smaller babies.
2. Low birth weight – refers to babies weighing less than 2,500 grams at birth (5 lbs, 8 oz.).
3. Very low birth weight – refers to babies weighing less than 1,500 grams or 3-4 lbs. at birth.
4. Pre-term labor – refers to the onset of labor before 37 weeks.
5. Despite educational and medical interventions geared towards the prevention and arrest of pre-term labor, it still remains a significant clinical problem and leads to high rates of infant mortality and morbidity.
For more information about pre-term infants, visit
http://www.marchofdimes.com/home.asp
Prenatal Care
The health status of a woman prior to and during pregnancy is critically important for the health and well being of the woman, and for the outcome her pregnancy. However, in the United States and around the world, standards vary.
“Most of the antenatal (prenatal) care models currently in use around the world have not been subjected to rigorous scientific evaluation to determine their effectiveness. Despite a widespread desire to improve maternal care services, this lack of “hard” evidence has impeded the identification of effective interventions and thus the optimal allocation of resources. In developing countries, routinely recommended antenatal care programs are often poorly implemented and clinical visits can be irregular, with long waiting times and poor feedback to the women.” WHO Antenatal Care Randomized Trial, 2001.16
Comprehensive prenatal care (also know as antenatal care) is designed to:
- Provide baseline health assessments (i.e. blood pressure, Pap smear, height, weight), and screenings for medical conditions that increase pregnancy-related risks (i.e. cardiovascular disease, hypertension, anemia, diabetes, and sexually transmitted infections including HIV, and/or urinary tract infections).
- Identify maternal behaviors that may increase risk (i.e. smoking, poor nutrition, substance use, psychosocial stressors, and unprotected sex), and initiate appropriate treatments.
- Provide genetic counseling.
- Provide health education focused on healthy nutrition/folic acid requirements, exercise, risk reduction, signs and symptoms of pre-term labor and/or other pregnancy complications that require immediate attention.
- Monitor the pregnancy to assure adequate weight gain, fetal growth, fetal heart beat, blood pressure control, assessment of fetal position (later in pregnancy), and assessment to exposure to environmental and infectious agents that can impact pregnancy.
- Identify risk factors for pre-term labor, treat conditions that may cause pre-term labor, and teach women the signs and symptoms of early labor, so that they may seek medical attention promptly.
- Identify maternal health and/or psychosocial factors that will require on-going post-pregnancy care (pregnancy and childbirth may motivate women to address physical and emotional health issues).
- Assess eligibility and provide referral for social welfare and entitlements programs available to the woman and her family.
In many developing countries, prenatal care consists of monitoring weight and blood pressure, measuring the fetal heartbeat, providing a tetanus toxoid immunization, administration of folic acid and iron, syphilis testing (rarely done), and birth planning for potential complications during delivery.
Childbirth
Labor and Delivery
Labor and delivery is the process that transports the fetus from the uterus through the vagina (birth canal) and results in the birth of a baby. Signs and symptoms of impending labor are: lightening (the descent of the fetal head into the pelvis), softening of the cervix, Braxton Hicks contractions (contractions which occur that have no measurable effect on the cervix), bloody show (the expulsion of a mucus plug from the cervix), a spurt of energy, and increased gastrointestinal discomfort. The presence of contractions, which become regular and increase in frequency, intensity and duration is an important sign that labor has begun.
Labor is divided into four stages, briefly described below:
First Stage
Regular contractions of the uterus cause the cervix to become thinner and the cervical os to open wider (dilation). Rupture of membranes (the amniotic sac containing the amniotic fluid breaks producing a gush of fluid) usually takes place during this phase. The first stage of labor continues from the onset of labor, until the dilation of the cervical os progresses to 10 cm.
Second Stage
In the second stage, the cervical opening has completely dilated (to 10 cm.) Contractions last longer and are more frequent. The woman is instructed to “push” while she experiences contractions, which facilitates the passage of the fetus through the cervix, and into the vaginal canal. The fetal head descends as the woman pushes the baby with each contraction. When birth is imminent, the head of the fetus can be seen (crowning). The second stage ends with the delivery of the baby.
Third Stage
The delivery of the placenta, membranes of the amniotic sac, and the umbilical cord (sometimes referred to as the afterbirth) occur during the third stage. The uterus continues to contract, which results in the separation of the placenta from the uterine wall. Placental delivery normally takes place within five minutes of infant delivery.
Fourth Stage
Marking the beginning of the post-partum period, the fourth stage takes place between one and four hours immediately following the delivery of the placenta. During this time, contractions of the uterus close off the blood vessels leading to the site of placental attachment.
Obstetrical Management
There are many factors which contribute to decisions about obstetrical management during childbirth which include: maternal preference and health status, fetal maturity and health status, fetal position, the stage of labor, and maternal and fetal responses to the labor.
Interventions that monitor both fetal and maternal responses to labor include internal and external fetal heart rate monitoring, maternal blood pressure, and fetal scalp sampling.
Decisions about the use of pain medication and Pitocin (a synthetic hormone which enhances uterine contractions) are also made based on the clinical situation.
In the United States, many women take childbirth education classes in order to learn relaxation and breathing techniques learned during childbirth education classes. These techniques help to reduce anxiety and provide varying levels of pain relief.
At the time of delivery, the prenatal care provider may perform an episotomy, a surgical incision of the perineum (the area between the vagina and the anus) in order to prevent the tissues from tearing, and/or to expedite delivery. The incision is repaired following delivery.
A systemic review of the outcomes of routine episiotomy was published in JAMA in 2005, which concluded that the procedure does not demonstrate maternal benefits. In fact, the authors conclude that routine use more often causes injury rather than benefit to women. The study calls upon clinicians and other public health practitioners to track the prevalence of circumstances that do warrant use of episiotomy (i.e. fetal distress) and develop standards of care that optimize neonatal outcome and minimize maternal harm.17
A Cesarean Section (C-Section) is a surgical procedure that allows for the birth of a baby through the abdomen instead of the vagina. C-Sections are performed in instances where vaginal delivery presents an unreasonable risk to the mother and/or the fetus (i.e. placental abnormalities, fetal position, disproportion between the size of the fetus' head and the size the woman's pelvis, and other medical problems including known HIV infection under certain circumstances). Complications related to C-Section are higher than those related to vaginal delivery, as with any surgery. C-Sections should be reserved for circumstances where the benefits outweigh the risks.
Post-Partum Period
The post-partum period, also know as the puerperium, begins with the delivery of the placenta and last for six weeks following delivery. During this period, the uterus goes through a process called involution (reduction in the size of the uterus following childbirth). The uterus discharges a fluid called lochia (fluid containing blood and other fluids) for a period of two-to-three weeks. During the first two-to-three days, the lochia is red because it is filled with blood. As post-partum adjustment continues, the lochia becomes lighter in color.
Breastfeeding and Lactation
Lactation Process
Lactation, the normal physiologic response of all women following childbirth, causes the mammary glands (breasts) to secrete milk. Lactation involves both milk production and milk “let-down.” During pregnancy, the placenta secretes high levels of estrogen and progesterone to prepare the breasts for lactation. Following the delivery of the placenta, the sudden drop in estrogen and progesterone triggers the pituitary gland to produce the hormone prolactin that stimulates the production of milk. Infant suckling stimulates the posterior pituitary gland to produce the hormone oxytocin which allows milk to “let down” (a reflex resulting in the release of milk from the alveoli to the milk ducts of the breasts). Without continued infant suckling, milk production and let down will cease within one-2 weeks.
Mechanical methods (manual or electric pumping devices, and/or hand expression of milk) can also stimulate milk production in situations where breast feeding at birth is not possible due to maternal/newborn illness or separation. Breast pumping also enables women to breast feed infants after returning to work because women maintain an adequate milk supply and provide babies with “pumped” breast milk, if proper storage and handling of breast milk is feasible.
Benefits of Breast-feeding
Breast milk is an ideal source of nutrition for infants because it provides the baby with essential nutrients, increases immunity, may prevent the development of allergies, and helps to foster an emotional bond between the mother and newborn. Breast milk is readily available, inexpensive, and safe in most situations.
HIV infection can be transmitted from an HIV-positive woman to her baby through breast-feeding. Wherever possible, women are advised to learn their HIV status during pregnancy, so that they can make informed decisions about their pregnancy, their own health, and choices for infant feeding.
Women who are HIV-positive are advised not to breastfeed. However, in locations where the availability of clean water is limited, and/or the cost of infant formula is beyond the means of the family, HIV-positive new mothers face a difficult choice.
Unlike the United States, breast-feeding for prolonged periods is the norm in many parts of the developing world. Frequent and continuous breast-feeding without supplementation with formula or food can inhibit ovulation, which has a contraceptive effect. For women who exclusively breastfeed (breastfeed on demand), and have not yet menstruated, breast-feeding is about 98% effective in preventing pregnancy for six months post-partum. The longer a woman breastfeeds, the more likely the contraceptive benefits will wear off. In developing countries, breast-feeding plays a major role in prolonging birth intervals and reducing fertility.18
In the United States and other developed countries, breast-feeding plays a smaller role in contraception because fewer women breastfeed, and/or breastfeed continuously without supplementation using infant formula.

