 |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| The Harriet and Robert Heilbrunn Department of Population and Family Health |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
intro | reproductive anatomy and physiology | contraception | pregnancy, childbirth and lactation |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
SECTION V:
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Introduction | Causes of Maternal Mortality |
| Maternal Mortality |
Introduction
Complications of pregnancy and childbirth are the leading causes of morbidity (illness) and mortality (death) among women of reproductive age in developing countries. There are approximately 529,000 pregnancy-related deaths worldwide each year.
There is a direct relationship between maternal death and infant and child survival. Approximately 7 million babies die each year before their first birthday (infant mortality), and about 50% of these deaths (3.4 million) occur at the time of delivery or during the first week of life. Maternal death also leaves over one million children motherless, which increases the risk of death for these children 3-10 times during the first two years. 25, 26
The highest incidence of pregnancy-related death occurs in the poorest countries in the world (countries in Africa and Asia), with sub-Sahara African having the highest rates. It is estimated that the life-time risk of maternal death there is one in 16, compared to one in 2,800 in developed countries. Pregnancy is the leading cause of death for young women ages 15-19 in developing countries.27
The following definitions are important in understanding maternal mortality:
- Maternal Mortality death of a woman while she is pregnant, or within 42 days of termination of pregnancy regardless of the site or duration of the pregnancy.
- Maternal Mortality Ratio the number of maternal deaths per 100,000 live births per year. The numerator includes deaths to women during their pregnancy or in the first six weeks after delivery. This measure is used conventionally rather than a rate because it is more accurate to use live births rather than total number of women to calculate the risk of death from pregnancy and childbirth.
- Maternal Mortality Rate the number of maternal deaths per 100,000 women of reproductive age (15-49). This measures the impact of maternal deaths on the population of women as a whole but is generally not used in public health since not all women are at risk for maternal mortality—only those that are pregnant.
- Maternal Morbidity refers to serious disease, disability or physical damage caused by pregnancy-related complications.
- Lifetime Risk of Maternal Death the probability of dying as a result of pregnancy cumulative across pregnancies in a woman's life.
- Infant Mortality the risk of an infant dying within the first year of life.
Obtaining accurate maternal death data is challenging in the developing world because accurate vital statistics are not available in many areas (particularly rural areas), and because the majority of births take place outside of health facilities. Instead of using vital statistics to track pregnancy related deaths, survey data is used instead. Thus, these data significantly underestimate the actual number of pregnancy-associated deaths.
The World Health Organization, the United Nations' Children's Fund and the United Nations Population Fund have developed a system to adjust existing data and provide estimates for countries lacking reliable data on maternal mortality. The table below provides a comparison of maternal mortality statistics throughout the developing and developed world.
WHO/UNICEF/UNFPA Estimates of number of maternal deaths, lifetime risk and maternal mortality ratio, by MDG regions, for the year 2000.28 |
|||||
MDG region |
Number of maternal deaths * |
Lifetime risk of maternal deaths: |
Maternal |
||
World |
529,000 |
74 |
400 |
||
Developed regions* |
2,500 |
2,800 |
20 |
||
|
Europe |
1,700 |
2,400 |
24 |
|
Developing regions |
527,000 |
61 |
440 |
||
|
Africa |
251,000 |
20 |
830 |
|
|
|
Northern Africa |
4,600 |
210 |
130 |
|
|
Sub-Saharan Africa |
247,000 |
16 |
920 |
|
Latin America and the Caribbean |
22,000 |
160 |
190 |
|
|
Asia |
253,000 |
94 |
330 |
|
|
|
Eastern Asia |
11,000 |
840 |
55 |
|
|
South-central Asia |
207,000 |
46 |
520 |
|
|
South-eastern Asia |
25,000 |
140 |
210 |
|
|
Western Asia |
9,800 |
120 |
190 |
|
Oceania |
530 |
83 |
240 |
|
* includes Canada, United States of America, Japan, Australia and New Zealand. |
|||||
Causes of Maternal Mortality
The leading causes of maternal death are classified as direct or indirect. Direct Causes are those related to obstetric complications of pregnancy, labor and delivery, and the post-partum periods. Direct causes account for 80% of maternal death. Indirect causes are those relating to pre-existing medical conditions that may be aggravated by the physiologic demands of pregnancy. A brief overview of the leading causes of maternal death in the developing world follows.
Some causes of maternal mortality are the same in the developing and developed world however the prevalence is significantly lower in the developed world. In fact, according to Minino, et al, in the United States, only 0.06% of women with direct obstetric complications died in facilities. This is well below the maximum acceptable case fatality rate of 1% as per UN guidelines. The most frequent cause of death was complications predominantly in the puerperium (28%), which was followed by pre-eclampsia, and eclampsia (21%).29
Direct Causes
Note: These cannot be predicted.
Hemorrhage (uncontrolled bleeding)
- Accounts for approximately 25% of maternal deaths and is the single most serious risk to maternal health.
- Blood loss during pregnancy, labor, or post-partum.
- Can rapidly lead to death without medical intervention.
- Can be treated with blood transfusions, oxytocics (drugs which induce uterine contractions to stop bleeding), and/or manual removal of the placenta.
Sepsis (infection)
- Accounts for approximately 15% of maternal deaths.
- Related to poor hygiene and infection control during delivery or to the presence of untreated sexually transmitted infections during pregnancy.
- Can be prevented or managed with high standards for infection control, appropriate prenatal testing and treatment of maternal infection, and appropriate use of intravenous or intramuscular antibiotics during labor and post-partum period.
Hypertensive Disorders
- Accounts for approximately 12% of maternal deaths
- Pre-eclampsia (also know as toxemia of pregnancy) is characterized by hypertension (high blood pressure), proteinurea (protein in the urine, general edema (swelling), and sudden weight gain. If left untreated, can lead to eclampsia.
- Eclampsia is characterized by kidney failure, seizures, and coma during pregnancy or post-partum. Can lead to maternal and/or infant death.
- Pre-eclampsia can be identified in the prenatal period by monitoring blood pressure, screening urine for protein, and through physical assessment.
- Treatment available during childbirth includes the use of sedative or anti-convulsant drugs.
Prolonged or Obstructed Labor
- Accounts for 8% of maternal deaths.
- Caused by cephalopelvic disproportion (CPD), a disproportion between the size of the fetal head and the maternal pelvis; or by the position of the fetus at the time of delivery.
- Increased incidence among women with poor nutritional status
- Use of assisted vaginal delivery methods such as forceps, vacuum extractor, or performing a Caesarean Section can prevent adverse outcomes.
- CPD is the leading cause of obstetrical fistula
Unsafe Abortion
- Accounts for approximately 13% of maternal deaths.
- In some parts of the world unsafe abortion accounts for 1/3 of maternal deaths.
- Approximately 67,000 cases of abortion related deaths occur each year.
- Can be prevented by providing safe abortion, quality family planning services, and competent post-abortion care.
Indirect Causes
- Accounts for approximately 20% of maternal deaths.
- Pre-existing medical conditions such as anemia, malaria, hepatitis, heart disease, and HIV/AIDS can increase the risk of maternal death.
- Risk of adverse outcomes can be reduced through prenatal identification and treatment as well as the availability of appropriate basic emergency obstetric care (EmOC) at the time of delivery.
Maternal Morbidity
For every maternal death there are approximately thirty times as many cases of pregnancy related illness or disability. For example, obstetric fistula (an opening between the bladder and the vagina) is usually the result of obstructed labor. It causes incontinence (the inability to hold urine). Although fistulas are preventable with good obstetric care, they have tragic consequences for many women, who are often left abandoned and isolated.
Prevention of Maternal Mortality: Promoting Safe Motherhood
Maternal death is directly correlated with lack of access to quality obstetrical care, family planning services, abortion facilities, and post-abortion care.
The International Conference on Population Development (1994), the Fourth World Conference on Women in Beijing (1995), and the Millennium Development Goals recognize the prevention of maternal death as an international public health priority. The reduction of maternal mortality is a leading Millennium Development Goal (MDG), which calls for a 75% reduction in maternal mortality by the year 2015.
Since the majority of maternal deaths are directly related to complications of pregnancy, childbirth, and the immediate post-partum period, the most significant strategy is to assure the availability, quality, and utilization of emergency obstetric care (EMOC) and skilled attendants at the time of delivery. In some parts of the world, projects designed to reduce maternal mortality have been successful, however in other parts of the world (particularly Africa and Asia) the numbers have not improved.
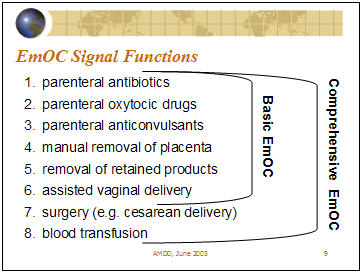
The components of basic and comprehensive EMOC are outlined below:
For more information about maternal mortality, visit:
- http://www.unfpa.org/mothers/facts.htm
- http://www.who.int/reproductive-health
/publications/maternal_mortality_2000/
For information about Emergency Obstetric Care in the United States, read:
- S. Lobis, D. Fry, A, Paxton, Program note: Applying the UN Process Indicators for Emergency Obstetric Care to the United States, International Journal of Gynecology and Obstetrics (2005) 88, 207-207.
continue to... Sexually Transmitted / Reproductive Tract Infections

