Assessing The Risk of Suicide
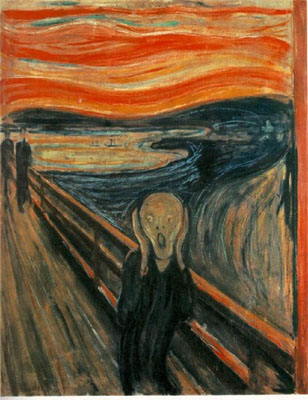
“The Scream” – Edvard Munch
Patients with depression may be at increased risk for suicide (Kahn, 1999. NYCDOH, 2006, Mann, 2005). Any patient that has a positive screening for depression should be evaluated for suicide risk. Asking about suicidal thoughts can save the patient’s life. Contrary to many physicians’ fear, asking about suicidal plans or ideation does not make patients more prone to commit suicide. Patients are usually relieved that they have been asked about their feelings and thoughts. Asking about suicidal ideation or plans conveys your interest in their well-being.
| Questions in Assessing Suicidal Risk |
|---|
|
Physicians can initiate the topic of suicidal ideation with questions about the patient’s feelings about life.
- “Did you ever wish you could go to sleep and never wake up?”
- “Have you ever felt life was not worth living?”
Depending on the response, more specific questions about suicidal ideation can be asked.
- “Do you ever feel others would be better off without you?”
- “Are you having thoughts about killing yourself?”
- “Have you thought about killing or hurting others?”
If suicidal ideation is elicited, physicians should ask patients if they have a suicidal plan (e.g., how, when, where). A patient that is actively thinking about suicide and has a plan for suicide constitutes a medical emergency. This is especially true in patients with previous suicide attempts. 911 should be called for safe transport to the nearest emergency room for psychiatric care. Prediction of which patients with suicidal ideation will attempt or commit suicide is very poor.
The Institute of Mental Health has made recommendations for physicians who are assisting potentially suicidal patients. It is important to monitor your own reactions to a suicidal patient. Stay calm and don’t appear threatened so that the patient feels secure and maintains the doctor-patient dialogue. Listen attentively so that the patient feels validated about their distress and is not ignored. Avoid judgmental statements. Emphasize that suicidal feelings worsen with stress, but is a treatable condition. Also highlight that suicide causes family members and friends great pain that lasts for years. Make it clear to the patient that he or she will have input into their treatment along with you and the psychiatric team as part of a partnership.
Outpatients at risk for suicide should not receive large supplies of antidepressants in case of overdose. Which one of the following statements is true about antidepressants and suicide? (Choose the best answer.)
A link to a recent article on whether antidepressants increase suicide risk and the advent of “black box” warnings is available in the library.