Medical Management of Depression
First line choices of antidepressant drugs
Which one of the following statements is true regarding the effectiveness of antidepressants agents for treating major depression? (Choose the best answer.)
Antidepressant medications’ effectiveness is generally comparable across classes and within classes of medications. The medications differ in side effect profiles, drug-drug interactions, and cost. The history of a positive response to a particular drug for an individual or a family member, as well as patient preferences, should also be taken into account. Most psychiatrists agree that an SSRI should be the first line choice. The dual action reuptake inhibitors venlafaxine and bupropion are generally regarded as second line agents. Tricyclics and other mixed or dual action inhibitors are third line, and MAOI’s (monoamine oxidase inhibitors) are usually medications of last resort for patients who have not responded to other medications, due to their low tolerability, dietary restrictions, and drug-drug interactions. Most primary care physicians would prefer that a psychiatrist manage patients requiring MAOI’s.
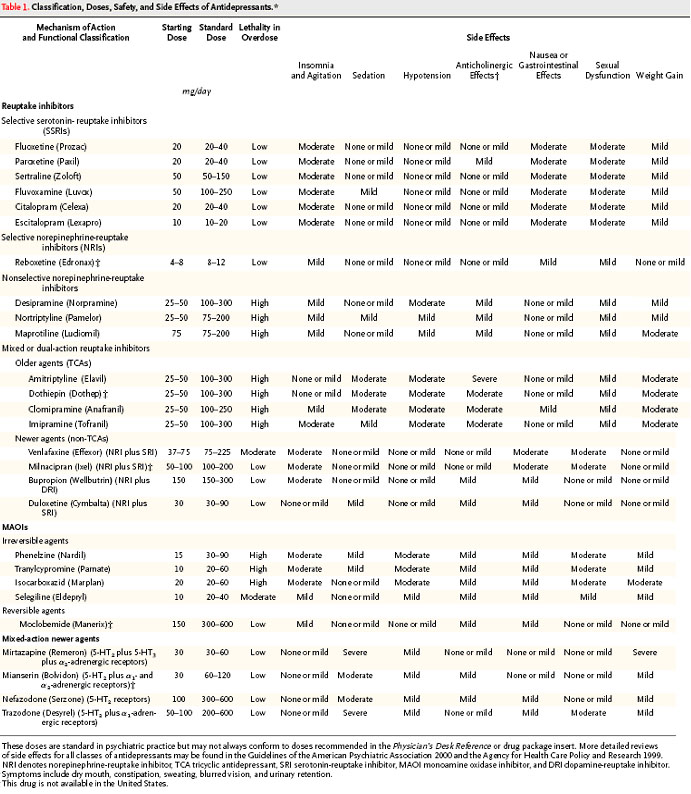
The recommended starting dose of antidepressants is illustrated in the table below from Mann JJ., “The Medical Management of Depression” New England Journal of Medicine. 2005 Oct 27;353(17):1819-34. Titration of the drug to therapeutic levels is done over the initial weeks of treatment. The rate of titration may depend on the patient’s age, the development of side effects, and comorbid conditions. In the geriatric population, the starting dose is usually half the recommended starting dose for other adults.
Classification, Doses, Safety, Side Effects of Antidepressants
Table reproduced with permission from the Massachusetts Medical Society. Taken from Mann, JJ., “The Medical Management of Depression” New England Journal of Medicine. 2005 Oct 27;353(17):1819-34. Copyright © 2005 Massachusetts Medical Society. All rights reserved.
Print Classification, Doses, Safety, Side Effects of Antidepressants Table
As stated prior, the patient should be monitored over time for improvement, exacerbation of depression, suicidal feelings, side effects, and adherence. All antidepressants may induce a manic episode in patients susceptible to bipolar disorder. The frequency of monitoring can vary from once a week to multiple times a week. Monitoring can be done via face-to-face visits, telephone contact via the physician and patient, or the patient and nursing staff. This can be a challenge in clinical practice, but there are novel approaches for improving systems for monitoring depressed patients in primary care settings (available in the library of this module).
Antidepressant Medications
Most antidepressant agents amplify norepinephrine or serotonin signaling by inhibiting their reuptake at the synaptic cleft.
Selective serotonin reuptake inhibitors (SSRIs)
Clinical trials have found little difference in efficacy and tolerability amongst the various SSRIs. SSRIs tend to be well tolerated as compared with other classes of antidepressants. The half life of all of the SSRIs is long enough to allow for once a day dosing, which improves patient adherence. Of note, fluoxetine is the only antidepressant found to be effective in controlled trials treating depressed children and adolescents. SSRIs have fewer cardiovascular effects than tricyclic antidepressants.
Tricyclic antidepressants (TCAs) and Norepinephrine reuptake inhibitors (NRIs)
TCAs and NRIs are older classes of antidepressants. They may be more effective in severe depression or depression with melancholic features. They may also be more effective than SSRIs for depression that has predominant physical symptoms or pain. TCAs and NRIs tend to have cardiac conduction effects and thus they are not the drug of choice in patients with cardiovascular conditions, particularly conduction defects. They are also contraindicated in people with benign prostatic hypertrophy, urinary retention, and closed angle glaucoma.
Dual action antidepressants
Venlafaxine, milnacipran, duloxetine are serotonin-norepinephrine reuptake inhibitors. They block monoamine transporters much more selectively than the TCAs and NRIs and thus have less cardiac-conduction effects. Venlafaxine has been shown to be more effective than SSRIs or TCAs through higher rates of remission in severe depression. Duloxetine is as effective as the SSRI paroxetine. Both duloxetine and paroxetine are also effective in treating chronic pain and diabetic neuropathy.
Bupropion inhibits norepinephrine and dopamine, but not serotonin, reuptake. It has similar efficacy to TCAs and SSRIs, but has less diarrhea, nausea, somnolescence, and sexual side effects than SSRIs. Bupropion also can be used as an adjunct in smoking cessation (although some health insurance companies will pay for buproprion as an antidepressant but not as a smoking cessation medication).
Monoamine oxidase inhibitors (MAOIs)
MAOIs nonselectively block Mao A and B isoenzymes, and have similar efficacy to TCAs. Again, MAOIs are not considered first line choice due to the side effect profile, drug-drug interactions, and the need to adhere to a low tyramine diet to prevent a hypertensive crisis. Under the care of a psychiatrist, MAOIs may be more effective than TCAs for atypical depression which is characterized by extreme fatigue, sensitivity to rejection, or troubled relationships.
Newer antidepressant therapies
Nefazodone blocks 5-HT serotonin receptors thus enhancing serotonin in synaptic clefts. It has an efficacy similar to SSRIs, and tends to be sedating.
Mirtazapine blocks alpha 2 – adrenergic receptors, specific serotonin receptors, and histamine receptors to enhance norepinephrine in the synaptic cleft. It is as effective as SSRIs and TCAs. Mirtazapine tends to be quite sedating and to cause significant weight gain.
Considerations before switching antidepressants
As mentioned prior, patients getting the same dose of an antidepressant and not achieving a response should consider having their antidepressant dose increased before changing the medication altogether. Before the medication is switched, the primary care physician should reassess the diagnosis; consider increasing the antidepressant dose; assess the patient for adherence; consider alcoholism or substance-abuse; and re-evaluate for coexisting medical conditions and use of non-psychiatric drugs that may contribute to treatment failure.
It is generally recommended that patients who don’t have a response to an SSRI should be switched to an antidepressant in another class. Similarly, if a dual action antidepressant has been used first, a switch to an SSRI should be considered. For patients with a partial response to one antidepressant, a second antidepressant from another class can be added for augmentation.
Adjunct medications
There are other medications that are used in conjunction with antidepressants to augment their effects. Mood stabilizers, such as lithium can prevent manic and depressive episodes in bipolar patients. Lithium can also be an effective augmenting agent in patients who don’t have an effective response to antidepressants alone. Antipsychotic medications can be added to antidepressants to treat depression with psychotic features.
Anxiety: Antidepressants and Anxiolytics
In major depression with comorbid anxiety or panic disorder (15 – 30% of cases), depression and anxiety symptoms resolve with antidepressant treatment. SSRIs and TCAs may initially worsen the anxiety. This can be avoided by starting at lower doses and titrating up more slowly.
Benzodiazepines are used as an adjuvant in 30 - 60% of cases of depression with anxiety or insomnia. Benzodiazepines improve antidepressant response, but can cause sedation, memory loss, and dependence and withdrawal syndromes. Benzodiazepines should be used on a limited basis to avoid dependency; avoided in those with a history of alcohol or drug abuse; and be used with extreme caution in geriatric populations who don’t metabolize the drugs well and can cause increased cognitive dysfunction, falls, and death. In general, benzodiazepines should not be used as the primary pharmacologic agent in any patient with major depression and anxiety disorders.